Foot and Ankle Conditions

BONE INFECTION
Osteomyelitis (an infection of the bone) can be caused by a variety of microbial agents (bacteria, fungus), the most common of which is staphylococcus aureus.
This serious infection can occur from a number of sources:
- It may enter bone through an injury, such as an open fracture with the bone ends piercing the skin.
- It can spread from elsewhere in the body or through the bloodstream.
- It can result from a chronic foot wound or infection, such as a diabetic ulcer.
To diagnose the condition, the foot and ankle surgeon will examine the area and may order blood tests and x-rays or other imaging studies. Treatment options include surgery, antibiotic therapy and hyperbaric oxygen therapy.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


BUNION
A bunion (also referred to as hallux valgus) is often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. The big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment—producing the bunion’s bump.
Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which becomes increasingly prominent. Symptoms usually appear at later stages, although some people never have symptoms.
Causes
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited but certain foot types that make a person prone to developing a bunion.
Although wearing shoes that crowd the toes will not actually cause bunions, it sometimes makes the deformity get progressively worse. Symptoms may therefore appear sooner.
Symptoms
Symptoms, which occur at the site of the bunion, may include:
- Pain or soreness
- Inflammation and redness
- A burning sensation
- Possible numbness
Diagnosis
Diagram indicating location of bunion on a footBunions are readily apparent—the prominence is visible at the base of the big toe or side of the foot. However, to fully evaluate the condition, the foot and ankle surgeon may take x-rays to determine the degree of the deformity and assess the changes that have occurred.
Because bunions are progressive, they do not go away and will usually get worse over time. But not all cases are alike—some bunions progress more rapidly than others. Once your surgeon has evaluated your bunion, a treatment plan can be developed that is suited to your needs.
Nonsurgical Treatment
Sometimes observation of the bunion is all that is needed. To reduce the chance of damage to the joint, periodic evaluation and x-rays by your foot care provider are advised.
In many other cases, however, some type of treatment is needed. Early treatments are aimed at easing the pain of bunions, but they will not reverse the deformity itself. These include:
Changes in shoewear. Wearing the right kind of shoes is very important. Choose shoes that have a wide toe box and forgo those with pointed toes or high heels, which may aggravate the condition.
Padding. Pads placed over the area of the bunion can help minimize pain. These can be obtained from your surgeon or purchased at a drug store.
Activity modifications. Avoid activity that causes bunion pain, including standing for long periods of time.
Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
Icing. Applying an ice pack several times a day helps reduce inflammation and pain.
Injection therapy. Although rarely used in bunion treatment, injections of corticosteroids may be useful in treating the inflamed bursa (fluid-filled sac located around a joint) sometimes seen with bunions.
Orthotic devices. In some cases, custom orthotic devices may be provided by the foot and ankle surgeon.
When Is Surgery Needed?
If nonsurgical treatments fail to relieve bunion pain and when the pain of a bunion interferes with daily activities, it is time to discuss surgical options with a foot and ankle surgeon. Together you can decide if surgery is best for you.
A variety of surgical procedures is available to treat bunions. The procedures are designed to remove the bump of bone, correct the changes in the bony structure of the foot and correct soft tissue changes that may also have occurred. The goal of surgery is the reduction of pain and deformity.
In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

BURSITIS
Bursitis is an inflammation of a small fluid-filled sac, called a bursa, located near a joint, bone or tendon. The bursa, which protects the area from friction, can become inflamed from repetitive motion or irritation from shoes. In the foot, the heel and the toes are most often affected.
Symptoms of bursitis include localized redness, swelling and pain. Treatment may include resting the affected area, local ice therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, padding or corticosteroid injections to help reduce inflammation and relieve pain. If these nonsurgical treatments fail to provide adequate pain relief, surgery may be needed.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

CALF PAIN
Calf pain can result from many different causes. Sometimes something as simple as overactivity causes muscle strain in the calf. Or dietary imbalances may cause cramping in the calf.
However, calf pain may be a symptom of more serious problems as well. Poor blood flow to the legs (peripheral vascular disease or PVD) may cause cramping in the calf while walking or when sitting with the legs elevated. A blood clot in the calf (deep vein thrombosis or DVT), a very serious problem, also produces pain in the calf.
Calf pain can also be the result of injuries, such as tearing of the calf muscle or tendonitis. In any case, it is not something that should be ignored. A foot and ankle surgeon should be seen for a thorough examination and diagnosis to determine whether the cause is due to a serious health problem, an injury or merely overuse. The cause of the calf pain will determine the proper treatment.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


COVID TOES
There’s been recent news coverage of “COVID toes” claiming certain rash or skin conditions can be linked to COVID-19. While we are still monitoring the correlation to the disease, foot and ankle surgeons do note that many viral conditions or other ailments can manifest in the feet, such as infected toenails, frost bite, or poor circulation from heart or lung disease. If you notice any changes to your feet, contact a foot and ankle surgeon for a proper consultation.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


CYST (GANGLION)
A ganglion cyst is a sac filled with a jellylike fluid that originates from a tendon sheath or joint capsule. The word “ganglion” means knot and is used to describe the knot-like mass or lump that forms below the surface of the skin.
Ganglion cysts are among the most common benign soft-tissue masses. Although they most often occur on the wrist, they also frequently develop on the foot—usually on the top, but elsewhere as well. Ganglion cysts vary in size, may get smaller and larger and may even disappear completely, only to return later.
Causes
Although the exact cause of ganglion cysts is unknown, they may arise from trauma—whether a single event or repetitive microtrauma.
Symptoms
A ganglion cyst is associated with one or more of the following symptoms:
- A noticeable lump—often this is the only symptom experienced
- Tingling or burning, if the cyst is touching a nerve
- Dull pain or ache, which may indicate the cyst is pressing against a tendon or joint
- Difficulty wearing shoes due to irritation between the lump and the shoe
Diagnosis
To diagnose a ganglion cyst, the foot and ankle surgeon will perform a thorough examination of the foot. The lump will be visually apparent, and, when pressed in a certain way, it should move freely underneath the skin. Sometimes the surgeon will shine a light through the cyst or remove a small amount of fluid from the cyst for evaluation. Your doctor may take an x-ray, and in some cases, additional imaging studies may be ordered.
Nonsurgical Treatment
There are various options for treating a ganglion cyst on the foot:
- Monitoring but no treatment. If the cyst causes no pain and does not interfere with walking, the surgeon may decide it is best to carefully watch the cyst over a period of time.
- Shoe modifications. Wearing shoes that do not rub the cyst or cause irritation may be advised. In addition, placing a pad inside the shoe may help reduce pressure against the cyst.
- Aspiration and injection. This technique involves draining the fluid and then injecting a steroid medication into the mass. More than one session may be needed. Although this approach is successful in some cases, in many others, the cyst returns.
When Is Surgery Needed?
When other treatment options fail or are not appropriate, the cyst may need to be surgically removed. While the recurrence rate associated with surgery is much lower than that experienced with aspiration and injection therapy, there are nevertheless cases in which the ganglion cyst returns.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.
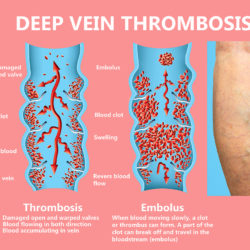
DEEP VEIN THROMBOSIS (DVT)
The blood supply of the leg is transported by arteries and veins. The arteries carry blood from the heart to the limbs; veins carry blood back to the heart. The leg contains superficial veins, which are close to the surface, and deep veins, which lie much deeper in the leg. Deep vein thrombosis (DVT) is a condition in which a blood clot (a blockage) forms in a deep vein. While these clots most commonly occur in the veins of the leg (the calf or thigh), they can also develop in other parts of the body.DVT can be very dangerous and is considered a medical emergency. If the clot (also known as a thrombus) breaks loose and travels through the bloodstream, it can lodge in the lung. This blockage in the lung, called a pulmonary embolism, can make it difficult to breathe and may even cause death. Blood clots in the thigh are more likely to cause a pulmonary embolism than those in the calf.
Causes of DVT
Many factors can contribute to the formation of a DVT. The more risk factors a person has, the greater the risk of having a DVT. However, even people without these risk factors can form a DVT.
Risk Factors for DVT:
- Blood or vein conditions:
- Previous DVT
- Varicose veins
- Blood clotting disorders
- Family history of DVT or blood clotting disorders
- Other medical conditions:
- Heart disease
- Chronic swelling of the legs
- Obesity
- Inflammatory bowel disease
- Cancer
- Dehydration
- Sepsis
Women’s health issues:
- Hormone replacement therapy
- Birth control pills containing estrogen
- Pregnancy or recent childbirth
Other:
- Age over 40 years old
- Immobility (through inactivity or from wearing a cast)
- Recent surgery
- Trauma (an injury)
- Smoking
Signs and Symptoms of DVT in the Leg
Some people with DVT in the leg have either no warning signs at all or very vague symptoms. If any of the following warning signs or symptoms are present, it is important to see a doctor for evaluation:
- Swelling in the leg
- Pain in the calf or thigh
- Warmth and redness of the leg
Diagnosis
DVT can be difficult to diagnose, especially if the patient has no symptoms. Diagnosis is also challenging because of the similarities between symptoms of DVT and those of other conditions, such as a pulled muscle, an infection, a clot in a superficial vein (thrombophlebitis), a fracture and arthritis. If DVT is suspected, the doctor will immediately send the patient to a vascular laboratory or a hospital for testing, which may include a blood test, Doppler ultrasound, venogram, MRI or angiogram.
Treatment of DVT
If tests indicate a clot is present, the doctor will make a recommendation regarding treatment. Depending on the location of the clot, the patient may need hospitalization. Medical or surgical care will be managed by a team of physicians, which may include a primary care physician, internist, vascular (blood vessel) surgeon or hematologist (blood disease specialist).
Treatment may include:
- Medication. A blood-thinning medication is usually prescribed to help prevent additional clots from forming.
- Compression stockings. Wearing fitted hosiery decreases pain and swelling.
- Surgery. A surgical procedure performed by a vascular specialist may be required.
- Complications of DVT
An early and extremely serious complication of DVT is a pulmonary embolism. A pulmonary embolism develops if the clot breaks loose and travels to the lung. Symptoms of a pulmonary embolism include:
- Shortness of breath
- Chest pain
- Coughing up blood
- A feeling of impending doom
A long-term consequence of DVT is damage to the vein from the clot. This damage often results in persistent swelling, pain and discoloration of the leg.
Preventive Measures
For those who have risk factors for DVT, these strategies may reduce the likelihood of developing a blood clot:
- Take blood-thinning medication, as prescribed by your medical provider.
- Reduce risk factors that can be changed. For example, stop smoking and lose excess weight.
- During periods of prolonged immobility, such as on long trips:
-
- Exercise legs every two to three hours to get the blood flowing back to the heart. Walk up and down the aisle of a plane or train, rotate ankles while sitting and take regular breaks on road trips.
- Stay hydrated by drinking plenty of fluids; avoid alcohol and caffeine.
- Consider wearing compression stockings.
-
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

DIABETIC PERIPHERAL NEUROPATHY
Diabetic neuropathy is nerve damage caused by diabetes. When it affects the arms, hands, legs and feet, it is known as diabetic peripheral neuropathy. Diabetic peripheral neuropathy is different from peripheral arterial disease (poor circulation), which affects the blood vessels rather than the nerves.Three different groups of nerves can be affected by diabetic neuropathy:
- Sensory nerves, which enable people to feel pain, temperature and other sensations
- Motor nerves, which control the muscles and give them their strength and tone
- Autonomic nerves, which allow the body to perform certain involuntary functions, such as sweating
Diabetic peripheral neuropathy does not emerge overnight. Instead, it usually develops slowly and worsens over time. Some patients have this condition long before they are diagnosed with diabetes. Having diabetes for several years may increase the likelihood of having diabetic neuropathy. The loss of sensation and other problems associated with nerve damage make a patient prone to developing skin ulcers (open sores) that can become infected and may not heal. This serious complication of diabetes can lead to loss of a foot, a leg or even a life.
Causes
The nerve damage that characterizes diabetic peripheral neuropathy is more common in patients with poorly managed diabetes. However, even patients living with diabetes who have excellent blood sugar (glucose) control can develop diabetic neuropathy. There are several theories as to why this occurs, including the possibilities that high blood glucose or constricted blood vessels produce damage to the nerves.
As diabetic peripheral neuropathy progresses, various nerves are affected. These damaged nerves can cause problems that encourage development of ulcers. For example:
- Deformities (such as bunions or hammertoes) resulting from motor neuropathy may cause shoes to rub against toes, creating a sore. The numbness caused by sensory neuropathy can make the patient unaware that this is happening.
- Because of numbness, a patient may not realize that s/he has stepped on a small object and cut the skin.
- Cracked skin caused by autonomic neuropathy, combined with sensory neuropathy’s numbness and problems associated with motor neuropathy, can lead to developing a sore.
Motor Neuropathy (Deformity) + Ill-Fitting Shoes + Sensory Neuropathy (numbness) = Ulcers (sores)
Symptoms
Depending on the type(s) of nerves involved, one or more symptoms may be present in diabetic peripheral neuropathy.
For sensory neuropathy:
- Numbness or tingling in the feet
- Pain or discomfort in the feet or legs, including prickly, sharp pain or burning feet
For motor neuropathy:
- Muscle weakness and loss of muscle tone in the feet and lower legs
- Loss of balance
- Changes in foot shape that can lead to areas of increased pressure
For autonomic neuropathy:
- Dry feet
- Cracked skin
Diagnosis
To diagnose diabetic peripheral neuropathy, the foot and ankle surgeon will obtain the patient’s history of symptoms and will perform simple in-office tests on the feet and legs. This evaluation may include assessment of the patient’s reflexes, ability to feel light touch and ability to feel vibration. In some cases, additional neurologic tests may be ordered.
Treatment
First and foremost, treatment of diabetic peripheral neuropathy centers on control of the patient’s blood sugar level. In addition, various options are used to treat the painful symptoms.
Medications are available to help relieve specific symptoms, such as tingling or burning. Sometimes a combination of different medications is used.
In some cases, the patient may also undergo physical therapy to help reduce balance problems or other symptoms.
Prevention
The patient plays a vital role in minimizing the risk of developing diabetic peripheral neuropathy and in preventing its possible consequences. Some important preventive measures include:
- Keep blood sugar levels under control.
- Wear well-fitting shoes to avoid getting sores.
- Inspect your feet every day. If you notice any cuts, redness, blisters or swelling, see your foot and ankle surgeon right away. This can prevent problems from becoming worse.
- Visit your foot and ankle surgeon on a regular basis for an examination to help prevent the foot complications of diabetes.
- Have periodic visits with your primary care physician or endocrinologist. The foot and ankle surgeon works together with these and other providers to prevent and treat complications from diabetes.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.



ORTHOTIC AND FOOTWEAR
Custom orthotics are medical devices prescribed by a foot and ankle surgeon. These are different from shoe inserts and arch supports in that they have two functions. Orthotics can be used to accommodate or offload a prominent area. This can be helpful for bursitis, calluses beneath bony prominences and ulcers. They can also help the foot function better in the case of hypermobility seen in tendonitis, fasciitis and other mechanically derived conditions. They can help support and align the foot and lower extremities as well. It is important how the foot shape or mold is captured, whether it be via laser scan, foam box or making a plaster cast.
Orthotics can help delay the need for surgery if it is not desired at a specific time. They can also help with pain following a surgery if an optimal result was not possible or achieved.
At this time, we do not prescribe custom orthotics. However, we can refer you to podiatrists in your area that can make them for you.
If cost is a factor, and you are seeking an alternative to non-custom orthotic, you can consider Protech Powerstep Orthotic brand.
You can order orthotics and supportive sandals at the website below and receive a 10% discount off your entire purchase.
Visit: www.powersteps.com/protech-Rx
Discount Code: 582a15ab
Footwear
The type of footwear you put on your feet can greatly impact the alignment of the bones in your feet, knees, hips, and lower back. It Is highly recommended that you wear supportive footwear that helps to prevent progression of foot deformity and alleviate foot pain.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.



PERIPHERAL ARTERIAL DISEASE
What Is Peripheral Arterial Disease?
Commonly referred to as poor circulation, Peripheral Arterial Disease (PAD) is the restriction of blood flow in the arteries of the leg. When arteries become narrowed by plaque (the accumulation of cholesterol and other materials on the walls of the arteries), the oxygen-rich blood flowing through the arteries cannot reach the legs and feet.
The presence of PAD may be an indication of more widespread arterial disease in the body that can affect the brain, causing stroke, or the heart, causing a heart attack.
Signs & Symptoms
Most people have no symptoms during the early stages of PAD. Often, by the time symptoms are noticed, the arteries are already significantly blocked.
Common symptoms of PAD include:
- Leg pain (cramping) that occurs while walking (intermittent claudication)
- Leg pain (cramping) that occurs while lying down (rest pain)
- Leg numbness or weakness
- Cold legs or feet
- Sores that will not heal on toes, feet or legs
- A change in leg color
- Loss of hair on the feet and legs
- Changes in toenail color and thickness
If any of these symptoms are present, it is important to discuss them with a foot and ankle surgeon. Left untreated, PAD can lead to debilitating and limb-threatening consequences.
PAD Risk Factors
Because only half of those with PAD actually experience symptoms, it is important that people with known risk factors be screened or tested for PAD.
The risk factors include:
- Being over age 50
- Smoking (currently or previously)
- Diabetes
- High blood pressure
- High cholesterol
- Personal or family history of PAD, heart disease, heart attack or stroke
- Sedentary lifestyle (infrequent or no exercise)
PAD Diagnosis
To diagnose PAD, the foot and ankle surgeon obtains a comprehensive medical history of the patient. The surgeon performs a lower extremity physical examination that includes evaluation of pulses, skin condition and foot deformities to determine the patient’s risk for PAD. If risk factors are present, the foot and ankle surgeon may order further tests.
Several noninvasive tests are available to assess PAD. The ankle-brachial index (ABI) is a simple test in which blood pressure is measured and compared at the arm and ankle levels. An abnormal ABI is a reliable indicator of underlying PAD and may prompt the foot and ankle surgeon to refer the patient to a vascular specialist for additional testing and treatment as necessary.
General Treatment of PAD
Treatment for PAD involves lifestyle changes, medication and, in some cases, surgery.
- Lifestyle changes. These include smoking cessation, regular exercise and a heart-healthy diet.
- Medications. Medicines may be used to improve blood flow, help prevent blood clots or control blood pressure, cholesterol and blood glucose levels.
- Surgery. In some patients, small incision (endovascular) procedures or open (bypass) surgery of the leg are needed to improve blood flow.
PAD & Foot Problems
Simple foot deformities (hammertoes, bunions, bony prominences) or dermatologic conditions, such as ingrown or thickened fungal nails, often become more serious concerns when PAD is present. Because the legs and feet of someone with PAD do not have normal blood flow—and because blood is necessary for healing—seemingly small problems, such as cuts, blisters or sores, can result in serious complications.
Having both diabetes and PAD further increases the potential for foot complications. People living with diabetes often have neuropathy (nerve damage that can cause numbness in the feet), so they do not feel pain when foot problems occur. When neuropathy occurs in people with PAD, ulcers can develop over foot deformities and may never heal. For this reason, PAD and diabetes are common causes of foot or leg amputations in the United States.
Once detected, PAD may be corrected or at least improved. The foot and ankle surgeon can then correct the underlying foot deformity to prevent future problems should the circulation become seriously restricted again.
Avoiding PAD Complications
Getting regular foot exams—as well as seeking immediate help when you notice changes in the feet—can keep small problems from worsening. PAD requires ongoing attention.
To avoid complications, people with this disease should follow these precautions:
- Wash your feet daily. Use warm (not hot) water and a mild soap. Dry your feet—including between the toes—gently and well.
- Keep the skin soft. For dry skin, apply a thin coat of lotion that does not contain alcohol. Apply over the top and bottom of your feet but not between the toes.
- Trim toenails straight across and file the edges. Keep edges rounded to avoid ingrown toenails, which can cause infections.
- Always wear shoes and socks. To avoid cuts and abrasions, never go barefoot—even indoors.
- Choose the right shoes and socks. When buying new shoes, have an expert make sure they fit well. At first, wear them for just a few hours daily to help prevent blisters and examine the feet afterward to check for areas of irritation. Wear seamless socks to avoid getting sores.
- Check your feet every day. Check all over for sores, cuts, bruises, breaks in the skin, rashes, corns, calluses, blisters, red spots, swelling, ingrown toenails, toenail infections or pain.
- Call your foot and ankle surgeon. If you develop any of the above problems, seek professional help immediately. Do not try to take care of cuts, sores or infections yourself.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


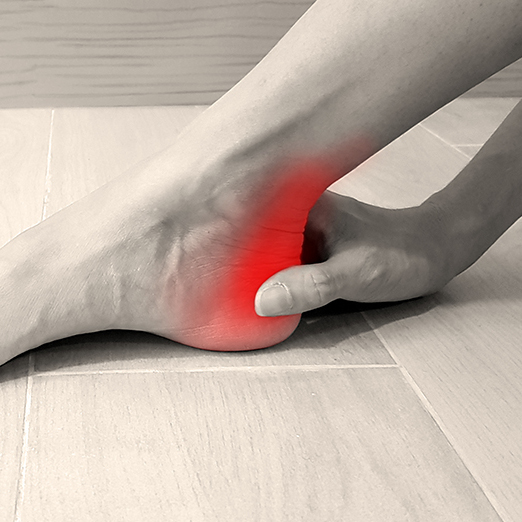
PLANTAR FASCIITIS (HEEL PAIN)
Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation or, rarely, a cyst.
Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and to determine the underlying source of your heel pain.
What Is Plantar Fasciitis?
Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
Causes
The most common cause of plantar fasciitis relates to faulty structure of the foot. For example, people who have problems with their arches, either overly flat feet or high-arched feet, are more prone to developing plantar fasciitis.
Wearing nonsupportive footwear on hard, flat surfaces puts abnormal strain on the plantar fascia and can also lead to plantar fasciitis. This is particularly evident when one’s job requires long hours on the feet. Obesity and overuse may also contribute to plantar fasciitis.
Symptoms
The symptoms of plantar fasciitis are:
- Pain on the bottom of the heel
- Pain in the arch of the foot
- Pain that is usually worse upon arising
- Pain that increases over a period of months
- Swelling on the bottom of the heel

People with plantar fasciitis often describe the pain as worse when they get up in the morning or after they have been sitting for long periods of time. After a few minutes of walking, the pain decreases because walking stretches the fascia. For some people, the pain subsides but returns after spending long periods of time on their feet.
Diagnosis
To arrive at a diagnosis, the podiatric provider will obtain your medical history and examine your foot. Throughout this process, the surgeon rules out all possible causes for your heel pain other than plantar fasciitis.
In addition, diagnostic imaging studies, such as x-rays or other imaging modalities, may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Nonsurgical Treatment
Treatment of plantar fasciitis begins with first-line strategies, which you can begin at home:
- Stretching exercises. Exercises that stretch out the calf muscles help ease pain and assist with recovery.
- Avoid going barefoot. When you walk without shoes, you put undue strain and stress on your plantar fascia.
- Ice. Putting an ice pack on your heel for 20 minutes several times a day helps reduce inflammation. Place a thin towel between the ice and your heel; do not apply ice directly to the skin.
- Limit activities. Cut down on extended physical activities to give your heel a rest.
- Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia.
- Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
If you still have pain after several weeks, see your podiatry provider, who may add one or more of these treatment approaches:
- Padding, taping and strapping. Placing pads in the shoe softens the impact of walking. Taping and strapping help support the foot and reduce strain on the fascia.
- Orthotic devices. Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the plantar fasciitis.

- Injection therapy. In some cases, corticosteroid injections are used to help reduce the inflammation and relieve pain.
- Removable walking cast. A removable walking cast may be used to keep your foot immobile for a few weeks to allow it to rest and heal.
- Night splint. Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients.

- Physical therapy. Exercises and other physical therapy measures may be used to help provide relief.
When Is Surgery Needed?
Although most patients with plantar fasciitis respond to nonsurgical treatment, a small percentage of patients may require surgery. If, after several months of nonsurgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
Long-Term Care
No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

PUNCTURE WOUNDS
What Is a Puncture Wound?
Puncture wounds are not the same as cuts. A puncture wound has a small entry hole caused by a pointed object, such as a nail that you have stepped on. In contrast, a cut is an open wound that produces a long tear in the skin. Puncture wounds require different treatment from cuts because these small holes in the skin can disguise serious injury.
Puncture wounds are common in the foot, especially in warm weather when people go barefoot. But even though they occur frequently, puncture wounds of the foot are often inadequately treated. If not properly treated, infection or other complications can develop.
Proper treatment within the first 24 hours is especially important with puncture wounds because they carry the danger of embedding the piercing object (foreign body) under the skin. Research shows that complications can be prevented if the patient seeks professional treatment right away.
Foreign Bodies in Puncture Wounds
A variety of foreign bodies can become embedded in a puncture wound. Nails, glass, toothpicks, sewing needles, insulin needles and seashells are some common ones. In addition, pieces of your own skin, sock and shoe can be forced into the wound during a puncture, along with dirt and debris from the object. All puncture wounds are dirty wounds because they involve penetration of an object that is not sterile. Anything that remains in the wound increases your chance of developing other problems, either in the near future or later.
Severity of Wounds
There are different ways of determining the severity of a puncture wound. Depth of the wound is one way to evaluate it. The deeper the puncture, the more likely it is that complications, such as infection, will develop. Many patients cannot judge how far their puncture extends into the foot. Therefore, if you have stepped on something and the skin was penetrated, seek treatment as soon as possible.
The type and cleanliness of the penetrating object also determine the severity of the wound. Larger or longer objects can penetrate deeper into the tissues, possibly causing more damage. The dirtier an object, such as a rusty nail, the more dirt and debris are dragged into the wound, increasing the chance of infection.
Another thing that can determine wound severity is if you were wearing socks and shoes, particles of which can get trapped in the wound.
Treatment
A puncture wound must be cleaned properly and monitored throughout the healing process to avoid complications.
Even if you have gone to an emergency room for immediate treatment of your puncture wound, see a foot and ankle surgeon for a thorough cleaning and careful follow-up. The sooner you do this, the better—within 24 hours after injury, if possible.
The surgeon will make sure the wound is properly cleaned and no foreign body remains. He or she may numb the area, thoroughly clean inside and outside the wound, and monitor your progress. In some cases, x-rays may be ordered to determine whether something remains in the wound or if bone damage has occurred. Antibiotics may be prescribed if necessary.
Avoiding Complications
Follow the podiatric provider’s instructions for care of the wound to prevent complications (see “Puncture Wounds: What You Should Do” further down on this page).
- Infection is a common complication of puncture wounds that can lead to serious consequences.
- Sometimes a minor skin infection evolves into a bone or joint infection, so you should look for these signs:
- A minor skin infection may develop two to five days after injury.
- The signs of a minor infection that show up around the wound include soreness, redness and possibly drainage, swelling and warmth. You may also develop a fever.
- If these signs have not improved, or if they reappear in 10 to 14 days, a serious infection in the joint or bone may have developed.
- Other complications that may arise from inadequate treatment of puncture wounds include painful scarring in the area of the wound or a hard cyst where the foreign body has remained in the wound.
- Although the complications of puncture wounds can be quite serious, early and proper treatment can play a crucial role in preventing them.
Puncture Wounds: What You Should Do
- Seek treatment right away. A Delay in care can increase your chance of infection.
- Get a tetanus shot if needed (usually every 10 years).
- See a podiatric provider within 24 hours.
- Follow your medical provider’s instructions.
- Keep your dressing dry.
- Keep weight off of the injured foot.
- Finish all your antibiotics (if prescribed).
- Take your temperature regularly. Watch for signs of infection (pain, redness, swelling, fever). Call your medical provider if these signs appear.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


Raynaud’s Phenomenon
Raynaud’s phenomenon is a condition that results in a bluish-white discoloration of fingers and toes, often as a result of exposure to cold. Stress, smoking and certain medications may trigger or worsen symptoms. The color change, which occurs from spasms in small blood vessels, becomes red and then returns to normal when blood flow resumes.
The condition most often affects women, with symptoms varying depending on the severity of the condition. Because there are no specific blood tests to diagnose this condition, the diagnosis is based on symptoms.
However, your doctor may order blood tests to determine whether the Raynaud’s phenomenon is associated with certain autoimmune diseases or other medical conditions.
Treatment for Raynaud’s phenomenon is aimed at prevention and protection of the toes and fingers.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


RHEUMATOID ARTHRITIS IN THE FOOT AND ANKLE
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a disease in which certain cells of the immune system malfunction and attack healthy joints.
RA causes inflammation in the lining (synovium) of joints, most often the joints of the hands and feet. The signs of inflammation can include pain, swelling, redness and a feeling of warmth around affected joints. In some patients, chronic inflammation results in damage to the cartilage and bones in the joint. Serious damage can lead to permanent joint destruction, deformity and disability.
When joints become inflamed due to RA, the synovium thickens and produces an excess of joint fluid. This overabundance of fluid, along with inflammatory chemicals released by the immune system, causes swelling and damage to the joint’s cartilage and bones.
Symptoms Affecting the Foot & Ankle
Foot problems caused by RA commonly occur in the forefoot (the ball of the foot, near the toes), although RA can also affect other areas of the foot and ankle. The most common signs and symptoms of RA-related foot problems, in addition to the abnormal appearance of deformities, are pain, swelling, joint stiffness and difficulty walking.
Deformities and conditions associated with RA may include:
- Rheumatoid nodules (lumps), which cause pain when they rub against shoes or, if they appear on the bottom of the foot, pain when walking
- Dislocated toe joints
- Hammertoes
- Bunions
- Heel pain
- Achilles tendon pain
- Flatfoot ankle pain
Diagnosis
RA is diagnosed on the basis of a clinical examination as well as blood tests.
To further evaluate the patient’s foot and ankle problems, the medical provider may order x-rays and/or other imaging tests.
Treatment by the Foot & Ankle Surgeon
While treatment of RA focuses on the medication prescribed by a patient’s primary provider or rheumatologist, the podiatric provider will develop a treatment plan aimed at relieving the pain of RA-related foot problems. The plan may include one or more of the following options:
- Orthotic devices. The surgeon often fits the patient with custom orthotic devices to provide cushioning for rheumatoid nodules, minimize pain when walking and give needed support to improve the foot’s mechanics.
- Accommodative shoes. These are used to relieve pressure and pain and to assist with walking.
- Aspiration of fluid. When inflammation flares up in a joint, the surgeon may aspirate (draw out) fluid to reduce the swelling and pain.
- Steroid injections. Injections of anti-inflammatory medication may be applied directly to an inflamed joint or to a rheumatoid nodule.
When Is Surgery Needed?
When RA produces pain and deformity in the foot that is not relieved through other treatments, surgery may be required. The foot and ankle surgeon will select the procedure best suited to the patient’s condition and lifestyle.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

STAPH INFECTIONS OF THE FOOT
Staphylococcus aureus is a type of bacteria that can be spread through the skin or open wound contact and is known to cause serious illness and infection if contracted. In recent years, certain types of staph bacteria, such as drug-resistant MRSA (methicillin-resistant Staphylococcus aureus), have become more common in high-traffic community areas, such as pool decks, locker rooms and schools. Those walking barefoot and suffering from common, relatively minor foot problems, such as cuts, cracks in the skin, athlete’s foot, eczema, ingrown toenails, puncture wounds or corns and calluses, can be at higher risk for infection. These conditions can cause minor tears in the skin, which can act as portals for the bacteria to enter the body.
Podiatric providers recommend simple steps to help prevent community-associated MRSA infections:
- Wash and bandage cuts.
- See a medical provider within 24 hours for any puncture wound.
- Never perform “bathroom surgeries” to cut or dig out an ingrown toenail.
- Keep feet clean and dry to prevent fungal infections, such as athlete’s foot.
If you have a cut or scrape that becomes red or swollen and is not healing in a timely manner, do not hesitate to see a podiatric provider for an examination.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.


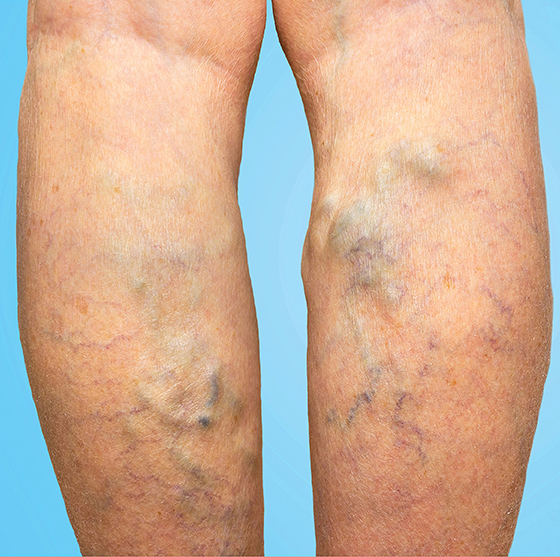
SWOLLEN FEET AND ANKLES
What causes edema?
Swelling of the ankles and feet may be due to many factors, some examples are listed below.
- Swelling can develop from weakened valves in the veins. Making it harder for the veins to push blood back to the heart.
- The build of fluid in the legs causes a condition called varicose veins.
- Certain diseases like peripheral vascular disease (PVD), congestive heart failure (CHF), kidney disease, pulmonary (lung) disease, thyroid disease can cause or make swelling in the foot worse.
- Some medications can cause swelling or make it worse. For example, calcium channel blocker.
- Too much salt in your diet, an allergic reaction, burns, trauma, poor nutrition can also cause or make swelling worse.
- Being pregnant can cause swelling in the legs as the uterus puts pressure on the blood vessels in the lower legs.
- Gravity can lead to swelling in the foot and ankle. This occurs when a person sits or stands for prolong periods.
- Other causes may include infection, blood clot in lower leg, tumor, or improper function of the lymphatic system.
Symptoms Include:
- Skin over the swollen area is shiny and appears stretched.
- Dimple forming after pressing over swollen area.
- Trouble walking if your lower extremities are also swollen.
- Coughing or trouble breathing if you have swelling in the lungs.
- Color changes to the skin in the leg
- Feeling of tightness and heaviness in the foot
- Thickening of the skin
Treatment:
- If the cause is related to a medication, stopping the medication will cause the swelling to resolve. It is very important to talk to your doctor before stopping any medication.
- Ask your doctor about reducing salt intake and drinking plenty of water if you have no fluid restrictions
- Wear support stockings/socks which prevents fluids from building up in your legs, foot and ankle. Click Donning on Socks (link it to the patient education sub-page) to access how to apply socks safely and easily.
- Your doctor may prescribe a diuretic (water pill) to help remove excess fluid from your body.
- Elevate your legs above the level of your heart, when lying down or sitting for prolonged periods. Gravity will help to return the blood back to your heart. It’s also important to move.
- If swelling is due to trauma like a sprained ankle or fracture using ice, or compression bandage can help reduce the swelling. If it does not go away, it is important that you call your medical provider or foot care provider to have an evaluation.
Important tip: Monitor swollen foot and ankle for any injury to the skin. Prolong swelling to the feet may result in skin infection or development of venous ulcers. Venous ulcers are slow to heal, it is important to identify them early to prevent worsening disease.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

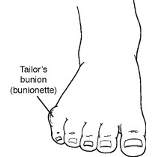
TAILORS BUNION (BUNIONETTE)
What Is a Tailor’s Bunion?
Tailor’s bunion, also called a bunionette, is a prominence of the fifth metatarsal bone at the base of the little toe. The metatarsals are the five long bones of the foot. The prominence that characterizes a tailor’s bunion occurs at the metatarsal head, located at the far end of the bone where it meets the toe. Tailor’s bunions are not as common as bunions, which occur on the inside of the foot, but they are similar in symptoms and causes.
Why is it called a tailor’s bunion? The deformity received its name centuries ago, when tailors sat cross-legged all day with the outside edge of their feet rubbing on the ground. This constant rubbing led to a painful bump at the base of the little toe.
Causes
Often a tailor’s bunion is caused by an inherited faulty mechanical structure of the foot. In these cases, changes occur in the foot’s bony framework, resulting in the development of an enlargement. The fifth metatarsal bone starts to protrude outward, while the little toe moves inward. This shift creates a bump on the outside of the foot that becomes irritated whenever a shoe presses against it.
Sometimes a tailor’s bunion is actually a bony spur (an outgrowth of bone) on the side of the fifth metatarsal head.
Regardless of the cause, the symptoms of a tailor’s bunion are usually aggravated by wearing shoes that are too narrow in the toe, producing constant rubbing and pressure.
Symptoms
The symptoms of tailor’s bunions include redness, swelling and pain at the site of the enlargement. These symptoms occur when wearing shoes that rub against the enlargement, irritating the soft tissues underneath the skin and producing inflammation.
Diagnosis
Tailor’s bunion is easily diagnosed because the protrusion is visually apparent. X-rays may be ordered to help the foot and ankle surgeon determine the cause and extent of the deformity.
Nonsurgical Treatment
Treatment for tailor’s bunion typically begins with nonsurgical therapies. Your podiatric provider may select one or more of the following:
- Shoe modifications. Choose shoes that have a wide toe box, and avoid those with pointed toes or high heels.
- Padding. Bunionette pads placed over the area may help reduce pain.
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may help relieve the pain and inflammation.
- Icing. An ice pack may be applied to reduce pain and inflammation. Wrap the pack in a thin towel rather than placing ice directly on your skin.
- Injection therapy. Injections of corticosteroid may be used to treat the inflamed tissue around the joint.
- Orthotic devices. In some cases, custom orthotic devices may be provided by the podiatric provider.
When Is Surgery Needed?
Surgery is often considered when pain continues despite the above approaches. In selecting the procedure or combination of procedures for your case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.

WEBBED TOES
Syndactyly most commonly affects the second and third toes, but it can occur between any of the toes.
The cause of webbed toes is generally unknown, although it may be congenital (inherited) or it may be associated with other conditions. Surgery to separate the toes may be performed in select cases.
DISCLAIMER: MATERIAL ON THIS SITE IS BEING PROVIDED FOR EDUCATIONAL AND INFORMATION PURPOSES AND IS NOT MEANT TO REPLACE THE DIAGNOSIS OR CARE PROVIDED BY YOUR OWN MEDICAL PROFESSIONAL.
This information should not be used for diagnosing or treating a health problem or disease or prescribing any medication. Visit a health care professional to proceed with any treatment for a health problem.
Source: https://www.foothealthfacts.com